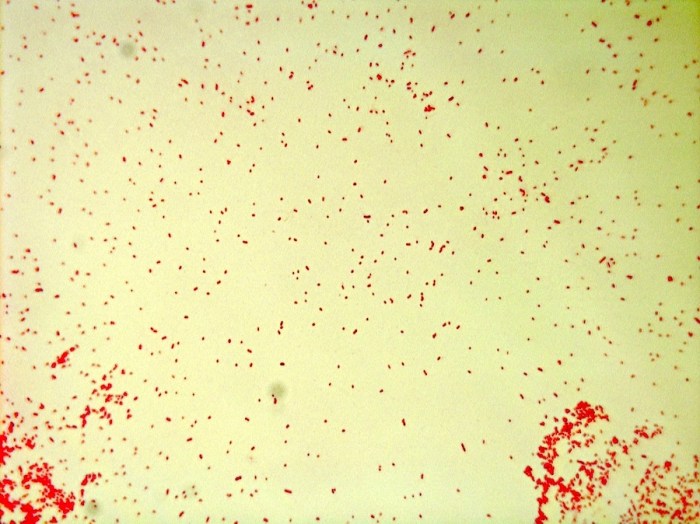
Serratia marcescens gram stain 1000x – The Gram stain, a cornerstone of microbiology, plays a pivotal role in identifying bacteria. In the realm of Gram-negative bacteria, Serratia marcescens stands out as a fascinating subject. This article delves into the intricate details of Serratia marcescens’ Gram staining characteristics under 1000x magnification, providing a comprehensive understanding of its morphology, cultural characteristics, pathogenicity, and clinical significance.
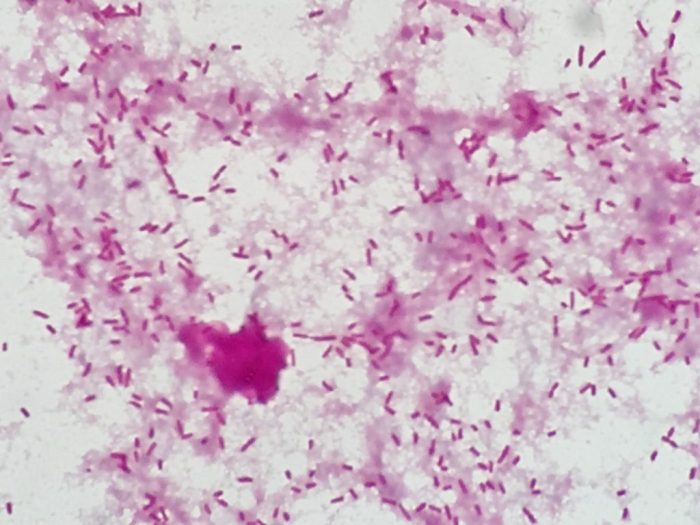
Serratia marcescens, a ubiquitous bacterium found in diverse environments, is renowned for its distinct red pigmentation. Its Gram-negative nature is a defining feature, rendering it susceptible to Gram staining. Under the microscope at 1000x magnification, Serratia marcescens appears as rod-shaped, Gram-negative bacteria, often arranged in pairs or short chains.
Morphology and Staining Characteristics: Serratia Marcescens Gram Stain 1000x
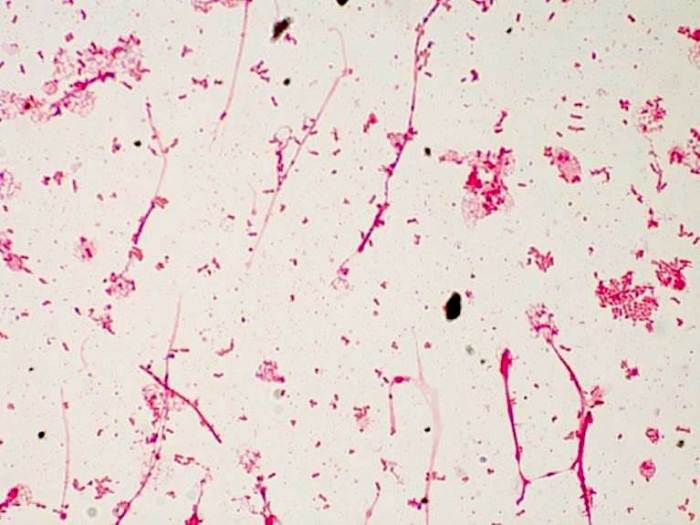
Serratia marcescens is a Gram-negative, rod-shaped bacterium that is typically 0.5-1.0 µm in width and 1.0-3.0 µm in length. It is a facultative anaerobe, meaning it can grow in both the presence and absence of oxygen.
The Gram staining procedure is a differential staining technique that is used to differentiate between Gram-positive and Gram-negative bacteria. Gram-positive bacteria have a thick peptidoglycan layer in their cell walls, which retains the crystal violet stain, causing them to appear purple.
Gram-negative bacteria have a thin peptidoglycan layer and an outer membrane, which prevents the crystal violet stain from penetrating, causing them to appear pink or red.
When Serratia marcescens is Gram stained, it will appear Gram-negative. This is because it has a thin peptidoglycan layer and an outer membrane, which prevents the crystal violet stain from penetrating. Under 1000x magnification, Serratia marcescens will appear as small, pink or red rods.
Cultural Characteristics
Serratia marcescens is a Gram-negative, facultative anaerobic bacterium that is commonly found in soil, water, and on plants. It is also an opportunistic pathogen that can cause infections in humans and other animals.
The optimal growth conditions for Serratia marcescens are a temperature of 25-30°C and a pH of 7.0-7.5. The bacterium can grow on a variety of culture media, including blood agar, MacConkey agar, and nutrient agar.
Colony Morphology
On blood agar, Serratia marcescens colonies are typically round, smooth, and non-hemolytic. On MacConkey agar, colonies are typically pink or red due to the bacterium’s ability to ferment lactose. On nutrient agar, colonies are typically cream-colored or slightly yellow.
Biochemical Tests
A variety of biochemical tests can be used to identify Serratia marcescens. These tests include the catalase test, the oxidase test, the indole test, the methyl red test, and the Voges-Proskauer test.
- Catalase test: Serratia marcescens is catalase-positive, meaning that it produces the enzyme catalase, which breaks down hydrogen peroxide into water and oxygen.
- Oxidase test: Serratia marcescens is oxidase-negative, meaning that it does not produce the enzyme cytochrome oxidase, which is involved in the electron transport chain.
- Indole test: Serratia marcescens is indole-positive, meaning that it produces the compound indole, which is a byproduct of the breakdown of tryptophan.
- Methyl red test: Serratia marcescens is methyl red-positive, meaning that it produces the compound methyl red, which is a byproduct of the fermentation of glucose.
- Voges-Proskauer test: Serratia marcescens is Voges-Proskauer-negative, meaning that it does not produce the compound acetoin, which is a byproduct of the fermentation of glucose.
Pathogenicity and Virulence Factors
Serratia marcescens is a Gram-negative bacterium that is widely distributed in the environment. It is an opportunistic pathogen, meaning that it can cause infections in individuals with weakened immune systems or underlying medical conditions. The virulence factors of S. marcescens contribute to its ability to cause disease.
Virulence Factors
- Proteases:S. marcescens produces a variety of proteases that can degrade host proteins and promote tissue invasion.
- Hemolysins:These proteins lyse red blood cells and contribute to the characteristic red pigmentation of S. marcescens colonies.
- Lipopolysaccharide (LPS):The LPS of S. marcescens is a major virulence factor that triggers inflammation and activates the host immune response.
- Biofilm formation:S. marcescens can form biofilms on medical devices and other surfaces, making it more difficult to treat infections.
Infections Caused by S. marcescens, Serratia marcescens gram stain 1000x
S. marcescens can cause a variety of infections, including:
- Urinary tract infections (UTIs)
- Pneumonia
- Skin and soft tissue infections
- Meningitis
- Sepsis
Antibiotic Resistance
S. marcescens is becoming increasingly resistant to antibiotics. This is due to several mechanisms, including:
- Efflux pumps:These pumps expel antibiotics from the bacterial cell, making them less effective.
- Beta-lactamases:These enzymes break down beta-lactam antibiotics, rendering them ineffective.
- Porin mutations:Mutations in porins, which are channels in the bacterial cell membrane, can prevent antibiotics from entering the cell.
The increasing antibiotic resistance of S. marcescens is a major concern, as it can make infections difficult to treat.
Clinical Significance
Serratia marcescens is a Gram-negative, opportunistic pathogen that can cause a wide range of infections in humans, particularly in immunocompromised individuals and those with underlying medical conditions.
Risk factors associated with Serratia marcescens infections include:
- Prolonged hospitalization
- Indwelling medical devices (e.g., catheters, ventilators)
- Weakened immune system (e.g., due to immunosuppressive therapy, HIV/AIDS)
- Exposure to contaminated water or medical equipment
Serratia marcescens can cause various infections, including:
- Pneumonia
- Urinary tract infections
- Skin and soft tissue infections
- Bacteremia
- Endocarditis
- Meningitis
Treatment of Serratia marcescens infections typically involves the use of antibiotics, such as fluoroquinolones, aminoglycosides, or carbapenems. The choice of antibiotic depends on the severity of the infection, the underlying medical condition of the patient, and the susceptibility of the organism to specific antibiotics.
Query Resolution
What is the clinical significance of Serratia marcescens?
Serratia marcescens is an opportunistic pathogen that can cause a wide range of infections, including urinary tract infections, respiratory tract infections, and bloodstream infections. It is particularly prevalent in healthcare settings, where it can lead to hospital-acquired infections.
How is Serratia marcescens treated?
Treatment for Serratia marcescens infections typically involves the use of antibiotics. The choice of antibiotic depends on the severity of the infection and the susceptibility of the bacteria to different antibiotics.
What are the risk factors for Serratia marcescens infections?
Risk factors for Serratia marcescens infections include weakened immune systems, prolonged hospital stays, and the use of invasive medical devices.